Why Do Babies Cry? The Anatomical and Physiological Changes During the Moments After Birth.
Smiles, relief, congratulations and applause do not start when a child is born – they start when it cries. Without crying, the room becomes increasingly silent and the mood increasingly apprehensive; and for good reason – crying is a very positive sign of a new, healthy life. Many factors and complex interactions go into the production of the sound that announces joyful, healthy childbirth.
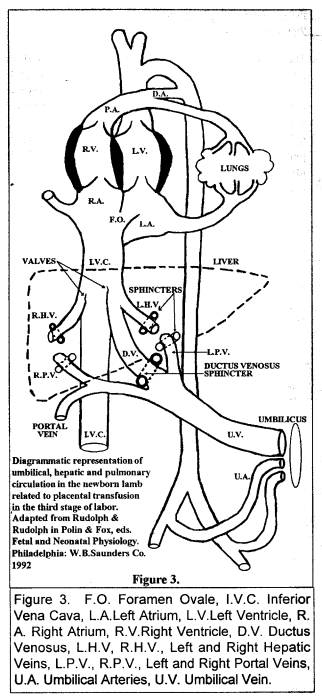
Fetal Circulation (Figure 3.)
Before birth, oxygenated blood from the placenta flows into the child’s inferior vena cava and mixes with blood returning from the lower part of the body. The atria are, in effect, one chamber due to the open foramen ovale; however, laminar blood flow tends to supply the left atrium and ventricle (and hence the upper body) with more placental (oxygenated) blood than the right atrium receives. The ventricles also act as one and pump blood around the body. Blood from the right ventricle bypasses the lungs, flowing through the ductus arteriosus and joining blood from the left ventricle in the descending aorta. A large portion of this blood flow goes to the placenta through the umbilical arteries.
Although the pulmonary vessels are fully developed in the fetus, only a tiny amount of blood (about 5% of cardiac output) flows through them due to intense vasoconstriction of the pulmonary arterioles. The nutritive blood supply to the lungs is from the bronchial arteries that arise from the aorta. The collapsed alveoli (air sacs) are filled with amniotic fluid.
Oxygenated blood is red, de-oxygenated blood is blue, and at the moment of birth, a normal newborn is circulating a mixture of blue and red blood. The color (lips and tongue) of a healthy newborn at birth is a pinkish purple; the child has been this color for nine months and normal placental function (cord pulsating) will maintain this color until the lungs function.
When the lungs are functioning, the umbilical vessels close, the ductus venosis closes, the hepatic portal vein is open, the foramen ovale closes, the heart is two sided, the cardiac output from the right ventricle (blue blood) goes through the lungs and is oxygenated, the left ventricular output (red blood) goes through the body, the ductus arteriosus closes, the pulmonary arterioles are open, the alveoli are full of air and the child turns from purple to pink. All of this complicated process is coordinated and controlled by the child’s reflexes; it usually happens within three or four minutes of birth. What makes it happen?
All babies are born soaking wet, and on meeting the atmosphere, the skin cools; this triggers two reflexes:
1. The cold crying reflex – cold, wet diapers produce the same result, crying.
2. The cold pressor reflex – cold skin raises blood pressure.
In order to cry, the child must first take a deep breath, and an inspiratory “gasp” is often the first sign, triggered by cold, that a child is going to cry or breathe. Contraction of the diaphragm and intercostal muscles increase thoracic volume and create negative intra-thoracic pressure. Once air is in the lungs, another reflex is triggered that relaxes the pulmonary arterioles; this causes an enormous increase in pulmonary blood flow.
The cold pressor reflex increases the blood pressure in the aorta, and this may be sufficient to reverse blood flow through the ductus arteriosus causing more blood to flow through the lungs.
The cord is also cooling, and the cord is a well-designed self-refrigerator. It has no skin and blubber to keep it warm like the child. It contains only the cord vessels surrounded by a watery gel, Wharton’s jelly, covered by a single layer of cells, the amnion. Water evaporation cools it rapidly, causing the vessels to constrict; this further helps to raise systemic blood pressure and to reverse ductus arteriosus flow.
At the same time, a large transfusion of placental blood is being forced into the child by gravity and/or by uterine contraction, greatly increasing cardiac output and pulmonary blood flow. The net result of these changes is a large amount of blood flowing into the left atrium from the lungs, which raises left atrial pressure and closes the foramen ovale – the heart changes from one-sided to two-sided. The lungs are now oxygenating blood that is pumped round the body by the left ventricle – the child turns pink.
If the child has not taken the first breath, or is depressed and cannot breathe, the massive increase in pulmonary blood flow generated by the placental transfusion may, of itself, initiate ventilation. Jaykka [1,2] showed that the fetal lungs are erectile tissues; by injecting serum through the pulmonary artery of excised animal fetal lungs, the engorged capillaries around the alveoli erected them and caused air to enter through the trachea. With establishment of pulmonary blood flow, the high colloid osmotic pressure of blood causes absorption of amniotic fluid from the alveoli and “dries out” the lungs, filling the “erected” alveoli with air.
Cold will eventually cause the cord vessels to close; however, a high arterial blood oxygen concentration is probably a key factor in umbilical artery closure – they close before the umbilical vein closes; it may also cause ductus arteriosus closure. After umbilical artery closure, the placental transfusion may continue through the cord vein in a very measured and controlled manner.
Figure 1 is a recording of a placental transfusion [3] obtained by placing the newborn at the level of the placenta, wrapped in a warm blanket, on a recording scales. It was obviously not a typical birth – the cord pulsated for 19 minutes, the placental transfusion (cord closure) was completed after 20 minutes, and the child started crying about ten minutes after birth! This picture is worth many more than a thousand words.
During the first nine minutes, the vertical lines (indicating newborn movement) on the recording are scant. The child, apart from kicking the bed once (there was obviously no distress), was lying very still and comfortable. There is no record of it breathing during this time, and the thin-line tracing contrasts with the thick “activity” tracing after crying started. Weight variation, influenced by uterine contractions, indicates that a virtual tidal wave of placental blood flow was adequately oxygenating the child in the absence of any obvious lung function. The warm blankets suppressed the cold crying reflex for at least nine minutes.
Marked vertical “activity” lines occur at the height of uterine contraction / transfusion peaks, and crying starts after one of these. Figure 3 illustrates that the placental transfusion may be delivered under very high pressure, and the activity lines (presumed discomfort) coincide with high-pressure distension of the newborn liver. Pain causes crying; the placental transfusion, by painfully distending the liver, may be a safe backup for the cold crying reflex.
Figure 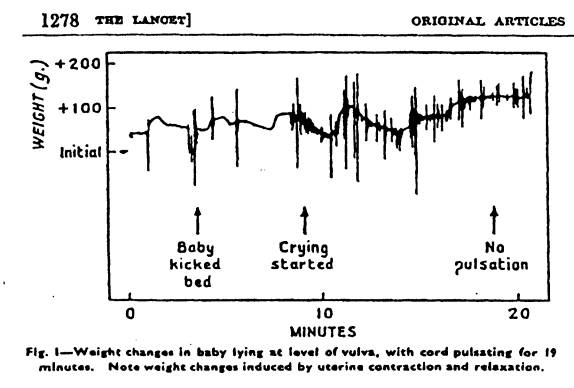
Figure 1. From Gunther M. The Transfer of Blood
Between the Baby and the Placenta.
Lancet 1957;I:1277-1280.
After crying starts, there is one contraction that injects nearly 100mls of blood into the child in less than one minute; the arteries pump it back into the placenta over the next three minutes. At the peak of this transfusion, not only the liver, but also the vena cava, the heart, the aorta and the pulmonary vessels are subjected to distension at arterial-like pressure. If Jaykka’s type of alveolar erection and aeration ever occurred in this child, it occurred during this uterine contraction. Thereafter, placental transfusion was under strict reflexive control, proceeding in a stepwise manner.
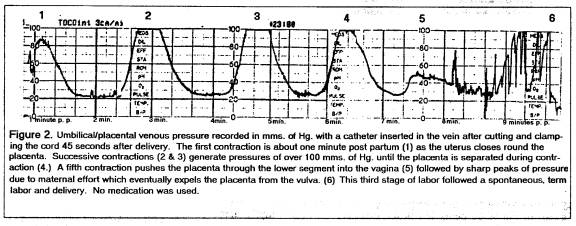
Figure 2.
If the patient had been in the natural squatting position for this delivery, the child, instead of being placed at the level of the placenta, would have been delivered downwards and would have been immediately subjected to a placental transfusion pressure 30+ cms. of water at birth due to gravity. Crying, (due to cold and liver pain) placental transfusion and cord closure would probably all have been completed within a minute or two.
The physiological mechanism that produces the “step” pattern is a sphincter-like closure of the umbilical vein that is reflexively controlled to work as a pressure valve. The right atrium has pressor receptors that are triggered by low central venous pressure; they control the release of anti-diuretic hormone. A pressor receptor in the left atrium that is triggered by adequate pressure to close the foramen ovale would be the ideal to effect closure of the umbilical vessels. Some cord pulsation was recorded at this time, but blood flow in the arteries was insignificant as there was no weight loss.
The first “step” indicates closure of the umbilical vein, followed by some relaxation of the closure while the blood volume increase is distributed throughout the child, but not enough relaxation to allow central venous pressure to cause blood loss into the placenta. The second uterine contraction “step” forces some blood volume past the relaxed “pressure valve,” triggering the final vein closure after the child has attained a maximal/optimal blood volume needed for healthy survival.
Dr. Gunther [3] recorded many similar “stepwise” placental transfusions; most were completed within three or four minutes. With an actively crying child and maximum gravity drainage (the child held well below the level of the placenta) the placental transfusion may be completed within 30 seconds.[4]
This reflexive closure of the umbilical vessels (arteries and vein) occurs in the portions of the vessels INSIDE the child’s abdomen. The blind remnants of these vessels become the two umbilical ligaments and the ligamentum teres of the liver in the adult. When natural cord closure is complete, the cord may be cut within a few inches of the umbilicus without clamping (this occurs routinely in every mammal except humans); no blood loss occurs from the child, but warm blood usually drains readily from the placental portion of the umbilical vein, indicating that additional placental transfusion was available if it had been needed. By this time, the umbilical arteries are constricted and empty.
The massive increase in blood volume from placental transfusion is soon decreased by hemo-concentration as fluid is transferred into the tissues; the hematocrit value rises, as does the albumin concentration. This increases plasma colloid osmotic pressure and keeps the lungs dry. Crying also keeps lungs dry by increasing alveolar air pressure. The normal weight loss that occurs after birth is mainly due to fluid being excreted through the kidneys; wet diapers soon after birth indicate that the child received a healthy placental transfusion.
As mentioned previously, cold, wet diapers trigger the cold, crying reflex. Mothers are not devoid of reflexes, and crying triggers the “baby pick-up” reflex. Crying babies don’t stay cold very long. Babies also cry because they are hungry, and mothers respond accordingly. The natural result of a crying child at birth should be its mother holding it while it is still attached to the placenta. In this situation, another maternal reflex is often demonstrated.
It is common practice nowadays for the cord to be doubly clamped while the child is on the mother’s abdomen and the scissors are handed to the parents to complete the job. Most mothers refuse, leaving it to the husband; some mothers recoil in horror, and if the cord is left intact, most mothers will not touch it. If they do, and especially if it is pulsating, the cord is treated as gently and tenderly as is a tiny finger or an ear of the child. New mothers are strongly inhibited from damaging the cord.
There are other stimuli that make a child breathe, and the most potent is asphyxia. The build up of carbon dioxide during asphyxia forces inspiratory efforts before oxygen lack becomes dangerous – try holding your breath for two minutes. Clamping a cord before the child is breathing will cause asphyxia and may force the child to breathe. Without placental transfusion, the child may breathe with lungs that have little blood flowing through them; such breathing will not reverse the asphyxia.
Some babies are born asphyxiated due to cord compression during birth, and are depressed to the extent that they do not respond to pain or cold or carbon dioxide. If the cord compression is relieved at birth, placental transfusion and placental oxygenation may correct the asphyxia and eventually restore the depressed reflexes. Artificial ventilation / resuscitation should always be conducted with the placental circulation intact.
All of the complex mechanisms in the changeover from placental oxygenation to pulmonary oxygenation have been programmed over millions of years into the human genome by natural selection to prevent and to relieve birth asphyxia. The primate brain is very large and very susceptible to permanent hypoxic damage; to ensure optimal survival of the individual, and of the primate order, natural closure of the umbilical cord must routinely provide perfect continuous oxygenation of the brain and routinely leave the newborn in optimal condition for survival. Disruption of the process with a cord clamp routinely harms the child.[5]
Use of Darwinian concepts and principles is not intended to cause dispute with Creationist convictions. Evolution provides a rational explanation of how variations in anatomy and physiology support life, [6] and why a fetus thrives in water without lungs, and with a fish-like heart, then changes within minutes into a crying, air-breathing mammal. A large, fragile brain distinguishes human (and primate) life, and a near perfect, innate mechanism to protect the brain during childbirth is essential for the continued existence of human life.
Dr. Crick, of double helix fame, once was reportedly asked how evolution could create anything as complex and brilliant as the human brain. He replied:
“Evolution is much more intelligent than you are.”
A new mother’s reflexes that inhibit her from damaging the newborn’s cord are much more sensible than a doctor wielding a cord clamp.
Something very intelligent designed the switch from placental to pulmonary respiration that makes a newborn baby cry, a creative work that is quite exquisite and marvelous regardless of one’s convictions about the nature of its Creator. That intelligence should be held in humble respect by evolutionists and creationists alike. It contrasts sharply with the ignorance and crass arrogance of those who would put a clamp on a pulsating umbilical cord.
G. M. Morley MB ChB FACOG
References:
- Jaykka S. Capillary Erection and Lung Expansion. Acta Paediatr. 1965 [nppl] 109.
- Jaykka S. An experimental study of the effect of liquid pressure applied to the capillary network of excised fetal lungs, Acta Paediatr. 1957; Supp 112:2-91.
- Gunther M. The transfer of blood between the baby and the placenta in the minutes after birth. Lancet 1957;I:1277-1280.
- Yao AC, Lind J. Effect of gravity on placental transfusion. Lancet, 1969; II:505-508
5.
“Another thing very injurious to the child, is the
tying and cutting of the navel string too soon; which should always be left
till the child has not only repeatedly breathed but till all pulsation in the
cord ceases. As otherwise the child is
much weaker than it ought to be, a portion of the blood being left in the placenta,
which ought to have been in the child.”
Erasmus Darwin, Zoonomia, 1801
- Charles Darwin M.A. On the Origin of Species by Means of Natural Selection. London: John Murray, Albermarle Street, 1859.
- Windle W. Brain Damage by Asphyxia at Birth. Scientific American. 1969 Oct;221(4):76-84.
Addendum:
Most of this article may be referenced in textbooks; many of the other details may be verified by carefully watching a physiological delivery performed by the mother. I have had several similar papers refused publication by the peer review press because of lack of data – the only specific data I have to offer is 40 years of obstetrical experience watching many newborns close their own cords, and watching other babies be snatched away to a resuscitation table past the outstretched arms and agonized face of a mother.
This study has few references on third-stage physiology because Gunther’s paper [gu] is the only valid scientific human study that I know of that has ever been published. In all other papers, and there are thousands of them, physiology has been disrupted with a cord clamp. None of these “cord clamp” papers has a physiological control set of newborns whose cords were not clamped and they are, therefore, scientifically invalid. “Late” clamping at five minutes may be claimed to be “physiological,” but on viewing Gunther’s included tracing, clamping at 5 minutes would have destroyed placental transfusion in that particular case; cord physiology does not obey the clock, it is controlled by other parameters.
Newborn birth defects such as RDS and hypoxic, ischemic brain damage do not occur naturally in other primates and this, some may argue, is due to other primates not resuscitating their offspring. However, these defects do occur in other primates when placental oxygenation and placental transfusion are artificially interrupted at birth and many of the neonates need resuscitation to survive. [7]
The highly advanced scientific obstetrical community and its peer reviewers have no data on babies that close their cords physiologically; most members regard the cord clamp as a normal newborn appendage and think that placental transfusion is harmful. However, the same type of data that was used by Charles Darwin [CD] in his publication is available – billions of successful, healthy births that occurred before the cord tie was ever thought of.
Obstetrical academia has massive amounts of data in the thousands of research papers on RDS, CP, neurological impairment, hyperviscosity, polycythemia and many other human newborn afflictions, real and imagined; all the thousands (millions?) of these afflicted newborns have one piece of data in common – all had their cords clamped. The profession, with all its data, has yet to prove that the cord clamp does anything other than injure the newborn.
Copyright G. M. Morley, April 11, 2002